
By Madeline O’Brien, Jack Hoadley, and Maanasa Kona
In January, the No Surprises Act (NSA) will provide landmark protections against surprise billing by shielding patients from expensive bills that typically occur after receipt of unanticipated out-of-network care, which is charged at a higher rate than in-network services. While the NSA applies to services provided by physicians, hospitals, ambulatory care centers, and air ambulances, ground ambulance services are excluded from the new protections. Ground ambulances are a major source of surprise bills: since consumers cannot choose an ambulance service when they dial 911, patients have limited ability to avoid out-of-network charges. At least half of all ground ambulance rides may result in a surprise bill, exposing consumers to out-of-network charges that exceed in-network charges by an average of $450.
In the absence of federal protections, several states have implemented surprise billing protections for ground ambulances. For state-regulated plans, ten states provide some protection for consumers from surprise bills by out-of-network ground ambulance services. Six of those states limit the amount a provider can bill the insurer for ground ambulance services.
In a new post for the Commonwealth Fund’s To the Point blog, CHIR’s Madeline O’Brien, Jack Hoadley, and Maanasa Kona discuss challenges related to ground ambulance reimbursement and state strategies for protecting consumers from surprise bills that may arise from emergency medical transportation. You can read the full post here. The table below provides additional detail on the ten state laws governing ground ambulance coverage and reimbursement.
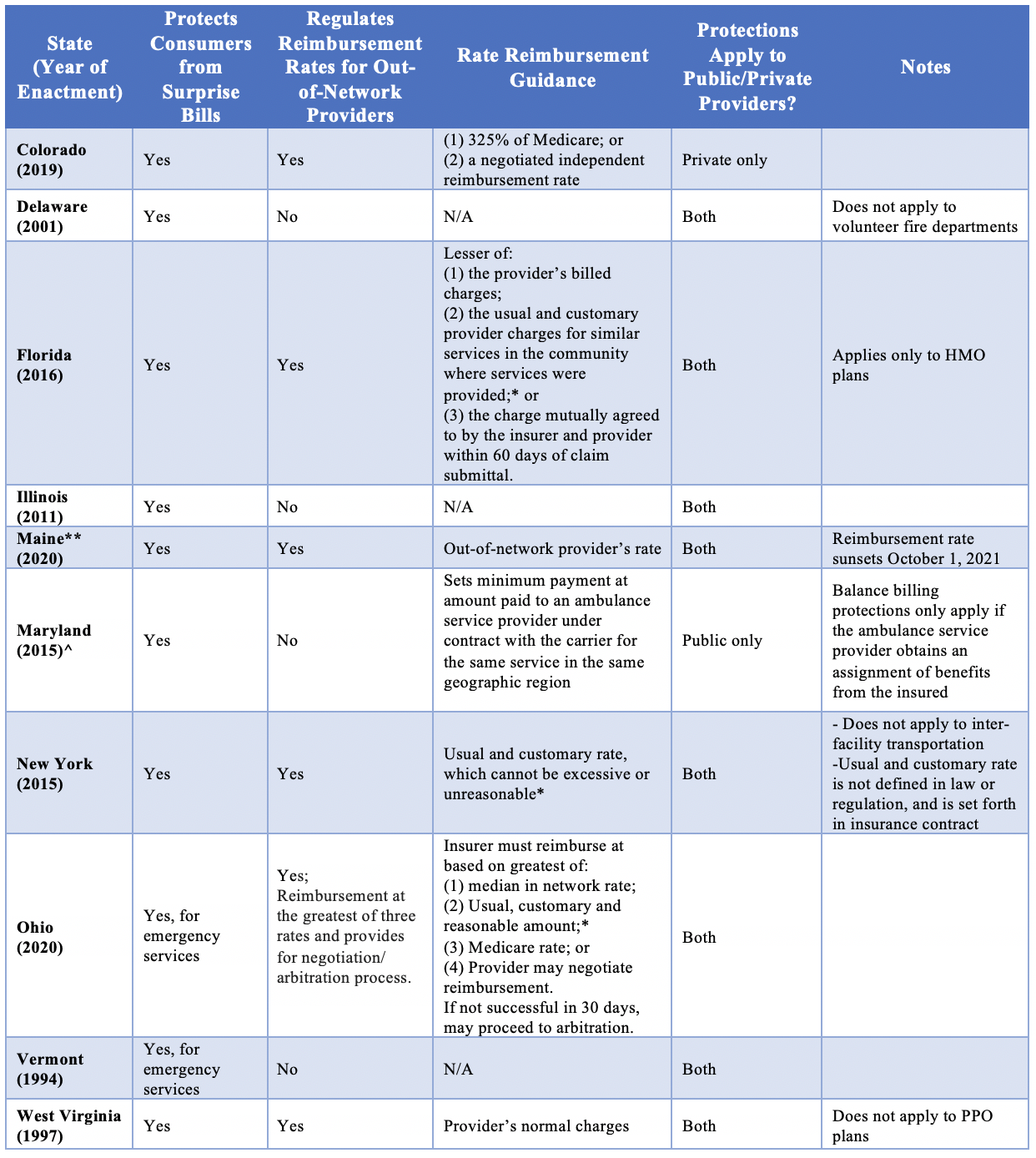
*Usual and customary amount can often end up close to the provider’s normal rate of billed charges.
**In 2021, Maine passed HP 925/LD 1258, which updates the reimbursement rate requirements for ground ambulance. Through December 2023, carriers are required to reimburse out-of-network providers at the lower of the provider’s rate or 180% of Medicare, plus any adjustments for transfer of Medicaid recipients by providers in rural or super-rural areas.
^Authors’ Note: An earlier version of the table in this piece stated that Maryland’s ground ambulance statute was enacted in 2020. It was enacted in 2015. We regret the error.


1 Comment
Thanks for the background story. I have been concerned about this ever since the Surprise Billing law excluded ambulance services.
The state regulations that you cite are frankly pathetic… easy to get around, and then there are 40 states with apparently no regulations.
The grown-up solution would be to consider ambulance service as a division of police and fire department work, and to provide federal funds to the providers.
There have to be some charges to the user so that the service is not used frivolously — maybe $150.
Covering the rest of the costs federally would be about $15 billion a year, which is a rounding error in health spending,