New Nationwide Data on Outpatient Facility Fee Reforms
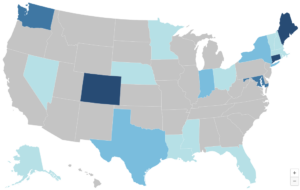
As hospitals and health systems expand their ownership and control of ambulatory care practices, they are frequently charging new facility fees for routine medical services delivered in outpatient settings. These bills are driving up premiums and health expenditures for consumers, employers, and, ultimately, tax payers. With support from and working in partnership with West Health, CHIR experts are studying outpatient facility fee billing reforms and share their findings in a new online repository.






