State And Federal Efforts To Improve Ownership Transparency

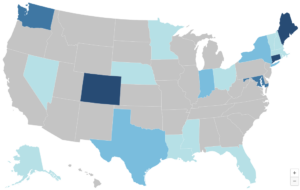
While there is some movement toward improved health care provider ownership transparency at the federal level and in some states, more attention is warranted given increasingly complex and obscured provider ownership structures and the impact they can have on health care prices, access, and quality. In a recent piece for Health Affairs Forefront, CHIR experts Stacey Pogue and Nadia Stovicek analyze efforts to improve ownership transparency at the state and federal levels.