By Dania Palanker and Nia Denise Gooding
The implementation of the Affordable Care Act (ACA) led to historic reductions in racial and ethnic disparities related to health insurance coverage. However, equal access to health coverage is not enough to ensure health equity. In the context of health coverage, health equity entails eliminating barriers that prevent all enrollees from living as healthy a life as possible. Federal and state-based marketplaces can take actions to increase health equity by implementing new policies such as requiring insurers to contract with essential community providers, requiring preventive care coverage, and prohibiting discriminatory health benefit design and other forms of discrimination.
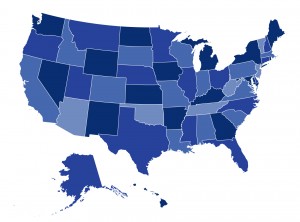
In their latest brief for the Commonwealth Fund, CHIR’s Dania Palanker and Nia Denise Gooding examine how four state-based health insurance marketplaces (California, Connecticut, the District of Columbia, and Massachusetts) have acted to reduce health inequity. The brief also outlines considerations for state-based marketplaces developing a health equity strategy, including opportunities and limitations under current law and information marketplaces need to best implement health equity plans. You can read the full issue brief here.

