Category: CHIR
New York Legislature Seeks to Control Outpatient Spending through Site-Neutral Payment and Rate Cap Proposal
Biden Administration Proposal to Improve Access to Free Preventive Services Faces Uncertain Future

The Biden Administration has proposed a rule to expand coverage of preventive services, including over-the-counter (OTC) contraceptives, without cost sharing. However, the proposal’s future is uncertain due to potential legal challenges and the political factors surrounding reproductive health. CHIR faculty Leila Sullivan and Amy Killelea discuss the proposal.
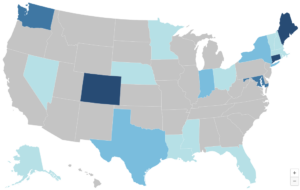
Enhancing Essential Health Benefits: How States Are Updating Benchmark Plans to Improve Coverage
The Affordable Care Act mandates that health plans in the individual and small-group markets cover essential health benefits (EHB), with states setting the scope through a benchmark plan. A new brief for the Commonwealth Fund by CHIR faculty explores how states have used recent flexibility to expand EHB, address consumer needs, and advance health policy, while highlighting ongoing challenges
Medicare Advantage and Medicare Part D: A New Compendium of Policy Proposals

In 2023, for the first time, more than half of Medicare beneficiaries were enrolled in Medicare Advantage (MA) plans, which offer private insurance alternatives to traditional Medicare, with 34 million enrollees in MA and 23 million in standalone Part D drug plans. A compendium of 70 policy proposals, created by Georgetown’s Center on Health Insurance Reforms, Medicare Policy Initiative offers a comprehensive resource for improving these programs, addressing issues like cost efficiency, provider networks, and many more.
Enhanced Premium Tax Credits Provide an Early Opportunity for Addressing Affordability Issues

Enhanced premium tax credits (PTCs) have significantly reduced health insurance premiums and expanded coverage for millions of Americans, particularly low- and middle-income individuals, but these subsidies are set to expire in 2025. If Congress doesn’t act to make them permanent, premiums will rise, leading to coverage losses and greater financial hardship for millions. CHIR’s Karen Davenport discusses what the incoming Congress can do to address healthcare affordability issues.
October Research Roundup: What We’re Reading

The leaves are falling but the latest health policy research is evergreen! Last month we read about health system competition in metropolitan areas, health care affordability prior to the American Rescue Plan (ARPA,) how high deductible health insurance can exacerbate racial and ethnic wealth disparities, and about unmet dental vision and hearing needs among low-income Medicare Advantage beneficiaries.
The Work Goes On: Preserving Equitable Access to Affordable, High Quality Health Insurance in Challenging Times
September Research Roundup: What We’re Reading

While the weather may be cooling down, the research is not! This month we read about Medicare Advantage quality bonus payments, out-of-pocket drug costs for consumers, effects of enhanced premium tax credits on older adults, and strategies to increase eligibility verification and receipt of Marketplace subsidies.
CHIR Expert Testifies About Facility Fees Before Texas House Insurance Committee
CHIR expert Christine Monahan recently testified before the Texas House Insurance Committee regarding outpatient facility fee billing. Her research highlights how facility fees contribute to significantly higher healthcare costs. In her testimony, she discussed measures to curtail hospital billing tactics that inflate costs and ways to mitigate financial burdens on patients.



